

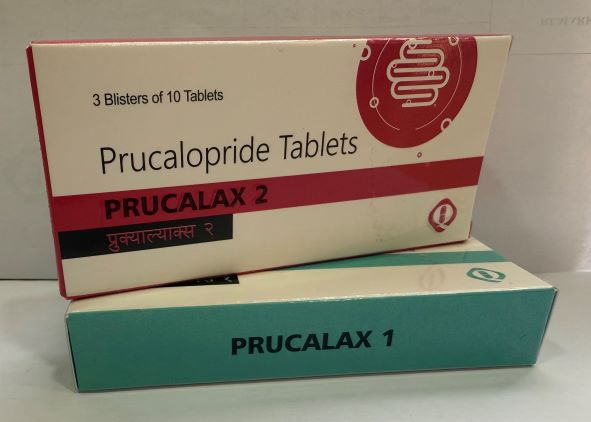
PRUCALAX
Film-Coated 1 /2 mg Tablet
Prucalopride (as succinate)
PRESENTATION
Dosage Form: Film Coated Tablets
Strength: 1/2 mg
Pack Size: 3*10
Packing: Blister
Group: KHA
CLINICAL PARTICULARS
Therapeutic Indications
PRUCALAX is indicated for the treatment of chronic functional constipation in adults in whom laxatives fail to provide adequate relief.
DOSE AND METHOD OF ADMINISTRATION
Dosage
PRUCALAX film-coated tablets are for oral use and can be taken with or without food.
Adults: 2 mg once daily.
Method of Administration
PRUCALAX film-coated tablets are for oral use and can be taken with or without food.
Dosage Adjustment
Hepatic Impairment
The dose for patients with severe hepatic impairment (Child-Pugh class C) is 1 mg once daily (see Special warnings and precautions for use and Pharmacokinetic properties). No dose adjustment is required for patients with mild to moderate hepatic impairment.
Due to the specific mode of action of PRUCALOPRIDE (stimulation of propulsive motility), exceeding the daily dose of 2 mg is not expected to increase efficacy.
Renal Impairment
The dose for patients with severe renal impairment not requiring dialysis (GFR < 30 mL/min/1.73m2) is 1 mg once daily (see Contraindications and Pharmacokinetic properties). No dose adjustment is required for patients with mild to moderate renal impairment.
Elderly (>65 Years)
Start with one 1 mg tablet once daily (see Pharmacokinetic properties); if needed the dose can be increased to 2 mg once daily.
Pediatric
PRUCALOPRIDE is not recommended in children and adolescents younger than 18 years.
Treatment Duration
If the intake of the prescribed once daily dose of PRUCALOPRIDE is not effective after four weeks of treatment, the patient should be re-examined and the benefit of continuing treatment should be reconsidered.
Efficacy and safety of PRUCALOPRIDE has been established in double-blind placebo controlled studies for up to 12 weeks. Patients should be reassessed after 12 weeks prior to continuation of treatment with Prucalopride.
Use with Laxatives
Efficacy and safety of PRUCALOPRIDE when used in combination with laxatives has not been assessed, although laxatives were used as rescue medications in the pivotal clinical trials.
CONTRAINDICATIONS
SPECIAL WARNINGS AND PRECAUTIONS FOR USE
Prior to receiving PRUCALOPRIDE patients require a thorough history and examination to exclude secondary causes of constipation and to establish failure to respond adequately to at least 2 different types of laxatives from different classes for at least 6 months.
The safety and efficacy of PRUCALOPRIDE in combination with laxatives has not been assessed, although laxatives were used as rescue medications in the pivotal clinical trials.
Secondary Constipation
Efficacy and safety of PRUCALOPRIDE has been demonstrated only in patients with chronic functional constipation. Efficacy and safety of PRUCALOPRIDE in patients with secondary causes of constipation including endocrine disorders, metabolic disorders and neurologic disorders have not been assessed and use in these patients is not recommended. Efficacy and safety of PRUCALOPRIDE in patients with medication-related constipation, including constipation due to opioid use as a secondary cause of constipation, has not been demonstrated and use of PRUCALOPRIDE is not recommended.
Concomitant Disease
There is limited information in patients with severe and clinically unstable concomitant disease (e.g. liver, cardiovascular or lung disease, neurological or psychiatric disorders, cancer or AIDS and other endocrine disorders). Therefore, caution should be exercised when prescribing PRUCALOPRIDE to patients with these conditions. In particular, PRUCALOPRIDE should be used with caution in patients with a history of arrhythmias or ischemic cardiovascular disease.
Oral Contraceptives
In case of severe diarrhea, the efficacy of oral contraceptives may be reduced and the use of an additional contraceptive method is recommended to prevent possible failure of oral contraception (see the prescribing information of the oral contraceptive).
Psychiatric Disorders
Suicides, suicide attempts, and suicidal ideation have been reported in clinical trials and post-market experience. A causal association between treatment with PRUCALOPRIDE and suicidal ideation and behavior has not been established. Patients should be monitored for persistent worsening of depression or the emergence of suicidal thoughts and behaviors.
Counsel the patients and their caregivers and family members to be aware of any unusual changes in mood or behavior, and to discontinue PRUCALOPRIDE and alert the healthcare provider immediately.
Use in Hepatic Impairment
A lower dose is recommended for patients with severe hepatic impairment (see Dose and method of administration).
Use in Renal Impairment
Renal excretion is the main route of elimination of Prucalopride (see Pharmacokinetic properties). A dose of 1 mg is recommended in subjects with severe renal impairment (see Dose and method of administration).
Use in the Elderly
Start with one 1 mg tablet once daily (see Dose and method of administration and Pharmacokinetic properties). If needed, the dose can be increased to 2 mg once daily.
Pediatric Use
PRUCALOPRIDE is not recommended in children and adolescents younger than 18 years.
Effects on Laboratory Tests
No effects are known.
INTERACTIONS WITH OTHER MEDICINES AND OTHER FORMS OF
INTERACTIONS
Potentiation of Effect
Ketoconazole (200 mg b.i.d.), a potent inhibitor of CYP3A4 and of P-gp, increased the area under the curve (AUC) of Prucalopride by approximately 40%. This effect is too small to be clinically relevant and is likely attributable to inhibition of P-gp mediated renal transport.
Interactions of similar magnitude as observed with ketoconazole may also occur with other
Potent inhibitors of P-gp such as verapamil, cyclosporine A and quinidine. Prucalopride is likely also secreted via another renal transporter(s). Inhibition of all transporters involved in the active secretion of Prucalopride (including P-gp) may theoretically increase the exposure by up to 75%.
Reduction of Effect
Because of the mechanism of action, the use of atropine-like substances may reduce the 5-
HT4 receptor mediated effects of PRUCALOPRIDE.
In vitro data indicate that Prucalopride has a low interaction potential, and therapeutic concentrations of Prucalopride are not expected to affect the CYP-mediated metabolism of co-medicated medicinal products. Prucalopride is a weak substrate for P-glycoprotein (P-gp). Prucalopride is a weak in vitro inhibitor of P-gp and BCRP transporters, and it is not a significant inhibitor of OATP1B1, OATP1B3, OAT1, OAT3, BSEP and MRP2 transporters.
Studies in healthy subjects showed that there were no clinically relevant effects of PRUCALOPRIDE on the pharmacokinetics of warfarin, digoxin, alcohol, paroxetine and oral contraceptives. A 30% increase in the plasma concentrations of erythromycin was found during PRUCALOPRIDE co-treatment. The mechanism for this interaction is not fully known, but the available data support that this is the consequence of the high intrinsic variability in erythromycin kinetics, rather than a direct effect of PRUCALOPRIDE.
There are no data on the effect of Prucalopride on SSRIs other than paroxetine or of the effect of SSRIs on Prucalopride.
Therapeutic doses of probenecid, cimetidine, erythromycin and paroxetine did not affect the pharmacokinetics of Prucalopride.
PRUCALOPRIDE should be used with caution in patients receiving concomitant drugs known to cause QTc prolongation. Interactions with food have not been observed.
FERTILITY, PREGNANCY AND LACTATION
Effects on Fertility
There is no information on the effects of Prucalopride on human fertility. There were no adverse effects on the fertility of rats treated orally or subcutaneously with Prucalopride at doses up to 20 mg/kg/day, with estimated exposure about 100 times clinical exposure at the MRHD, based on AUC.
Use in Pregnancy
Category B1
Experience with PRUCALOPRIDE during pregnancy is limited. Cases of spontaneous abortion have been observed during clinical studies, although, in the presence of other risk factors, the relationship to PRUCALOPRIDE is unknown. PRUCALOPRIDE is not recommended during pregnancy, and women of childbearing potential should use effective contraception during treatment with PRUCALOPRIDE.
There was no evidence of teratogenicity in rats or rabbits treated with Prucalopride during the period of organogenesis at oral doses up to 80 mg/kg/day, (respective exposures about 400 times and 40 times the clinical exposure at the MRHD, based on AUC).
Use in Lactation
Prucalopride is excreted in breast milk. However, at therapeutic doses of PRUCALOPRIDE, no effects on the breastfed newborns/infants are anticipated. In the absence of human data in women who breastfed while taking PRUCALOPRIDE, it is not recommended to use PRUCALOPRIDE during breast-feeding.
Oral administration of Prucalopride to rats from early gestation to weaning at doses up to 80 mg/kg/day was associated with slightly reduced pup survival due to maternotoxicity, with estimated exposure at least 100 times clinical exposure at the MRHD, based on AUC.
EFFECTS ON ABILITY TO DRIVE AND USE MACHINES
No studies on the effects of PRUCALOPRIDE on the ability to drive and use machines have been performed. PRUCALOPRIDE has been associated with dizziness and fatigue particularly during the first day of treatment which may have an effect on driving and using machines
(See Adverse Effects (Undesirable effects)).
ADVERSE EFFECTS (UNDESIRABLE EFFECTS)
The following adverse reactions were reported in controlled clinical studies at the recommended dose of 2 mg with frequencies corresponding to
Very Common (≥ 1/10),
Common (≥ 1/100 to < 1/10),
Uncommon (> 1/1,000 to < 1/100),
Rare (> 1/10,000 to <
1/1,000) and
Very Rare (≤ 1/10,000).
Metabolism and Nutrition Disorders
Common: Decreased Appetite
Nervous System Disorders
Very Common: Headache
Common: Dizziness
Uncommon: Tremors, Migraine
Cardiac Disorders
Uncommon: Palpitations
Ear and Labyrinth Disorders
Uncommon: Vertigo
Gastrointestinal Disorders
Very Common: Nausea, Diarrhea, and Abdominal Pain
Common: Vomiting, Dyspepsia, Flatulence, Abnormal Bowel Sounds
Uncommon: Rectal Hemorrhage
Renal and Urinary Disorders
Common: Polyuria
General Disorders and Administration Site Conditions
Common: Fatigue
Injury, poisoning and procedural complications
Reproductive System and Breast Disorders
Cardiac Disorders
Uncommon: Fever, Malaise
OVERDOSE
In a study in healthy volunteers, treatment with PRUCALOPRIDE was well tolerated when given in an up-titrating scheme up to 20 mg once daily (10 times the recommended therapeutic dose). An overdose may result in symptoms resulting from an exaggeration of the medicinal product’s known pharmacodynamics effects and include headache, nausea and diarrhea.
Specific treatment is not available for PRUCALOPRIDE overdose. Should an overdose occur, the patient should be treated symptomatically and supportive measures instituted, as required. Extensive fluid loss by diarrhea or vomiting may require correction of electrolyte disturbances.
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics Properties
Mechanism of Action
Pharmacotherapeutic Group: Drugs acting on serotonin receptors, in subjects with chronic constipation, there was a reduction in small bowel transit time, an increase in gastric emptying and more rapid colonic filling. There was an increase in the frequency of bowel motions but no significant effect on colonic transit time.
PHARMACOKINETIC PROPERTIES
Absorption
Prucalopride is rapidly absorbed; after a single oral dose of 2 mg, Cmax was attained in 2-3 hours. The absolute oral bioavailability is >90%. Concomitant intake of food does not influence the oral bioavailability of Prucalopride.
Distribution
Prucalopride is extensively distributed and has a steady-state volume of distribution (Vdss) of 567 L. The plasma protein binding of Prucalopride is about 30%.
Metabolism
Metabolism is not the major route of elimination of Prucalopride. In vitro, human liver metabolism of Prucalopride is very slow and only minor amounts of metabolites are found.
In an oral dose study with radiolabelled Prucalopride in man, small amounts of eight metabolites were recovered in urine and faces. The major metabolite (R107504, formed by O-demethylation and oxidation of the resulting alcohol function to a carboxylic acid) accounted for less than 4% of the dose. Unchanged active substance made up about 85% of the total radioactivity in plasma and only R107504 was a minor plasma metabolite.
Excretion
A large fraction of the active substance is excreted unchanged (about 60% of the administered dose in urine and at least 6% in faces) via both passive filtration and active renal transporters (P-gp and BCRP). Renal excretion of unchanged Prucalopride involves both passive filtration and active secretion. The plasma clearance of Prucalopride averages 317 mL/min. Its terminal half-life is about one day. Steady-state is reached within three to four days. On once daily treatment with 2 mg Prucalopride, steady-state plasma concentrations fluctuate between trough and peak values of 2.5 and 7 ng/mL, respectively.
The accumulation ratio after once daily dosing ranged from 1.9 to 2.3. The pharmacokinetics of Prucalopride is dose-proportional within and beyond the therapeutic range (tested up to 20 mg). Prucalopride o.d. displays time-independent kinetics during prolonged treatment.
Special Populations
Population Pharmacokinetics
A population pharmacokinetic analysis showed that the apparent total clearance of Prucalopride was correlated with creatinine clearance, and that there was no additional effect of age, body weight, sex or race.
Elderly
After once daily dosing of 1 mg, peak plasma concentrations and AUC of Prucalopride in elderly subjects were 26% to 28% higher than in young adults. This effect can be attributed to a diminished renal function in the elderly.
Renal Impairment
Compared to subjects with normal renal function, plasma concentrations of Prucalopride after a single 2 mg dose were on average 25% and 51% higher in subjects with mild (ClCR 50-79 mL/min) and moderate (ClCR 25-49 mL/min) renal impairment, respectively. In subjects with severe renal impairment (ClCR ≤ 24 mL/min), plasma concentrations were 2.3 times the levels in healthy subjects.
Hepatic Impairment
Non-renal elimination contributes to about 35% of total elimination. After a single oral dose of 2mg, Cmax and AUC of Prucalopride were on average 10-20% higher in patients with moderate and severe hepatic impairment than in subjects with normal hepatic function.
Pediatric
After a single oral dose of 0.03 mg/kg in pediatric patients aged between 4 and 12 years, Cmax of Prucalopride was comparable to the Cmax in adults after a single 2 mg dose, while unbound Area under the Curve (AUC) was 30-40% lower than after 2mg in adults. Unbound exposure was similar over the whole age-range (4-12 years). The average terminal half-life in the pediatric subjects was about 19 hours (range 11.6 to 26.8 hours). PRUCALOPRIDE is not recommended in children or adolescents.
Special Precautions for Storage
PRUCALOPRIDE tablets should be kept out of reach of children. Store below 30°C. Protect from moisture.