

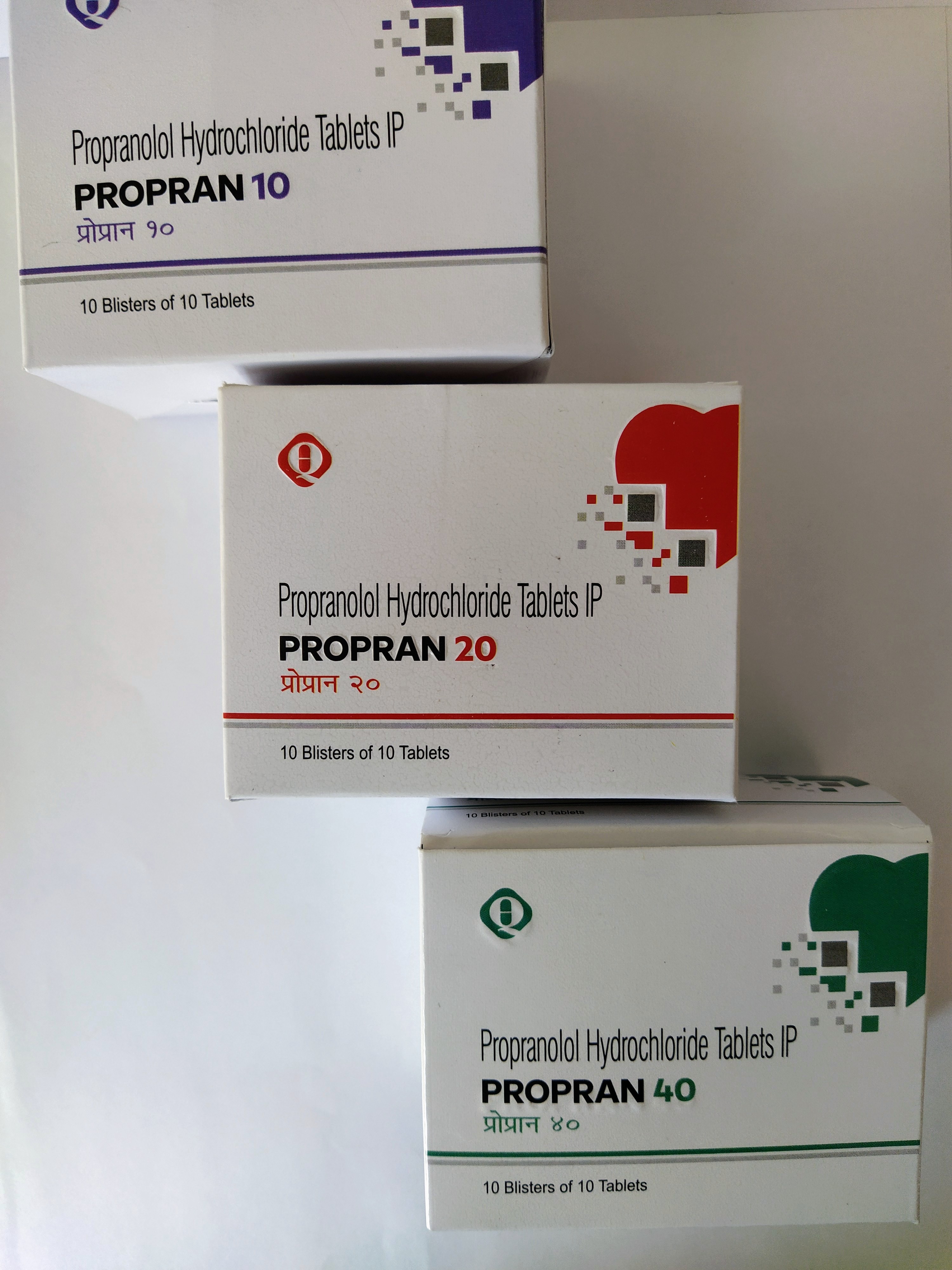
PROPRAN
Propranolol Hydrochloride 10/ 20/ 40 mg Un-coated Tablets
The active ingredients of the Propran is Propranolol. Propranolol is a non-selective beta adrenergic antagonist used to treat hypertension, angina, atrial fibrillation, myocardial infarction, migraine, essential tremor, hypertrophic sub aortic stenosis, and pheochromocytoma.
PRESENTATION
Each Uncoated Tablet Contains IP 10/ 20/ 40 mg.
Packing: Blister
Pack Size: 10*10
CLINICAL PARTICULARS
Therapeutic Indications
POSOLOGY AND METHOD OF ADMINISTRATION
POSOLOGY
Adults
Hypertension
A starting dose of 80 mg twice a day may be increased at weekly intervals according to response. The usual dose range is 160 to 320 mg per day. With concurrent diuretic or other antihypertensive drugs a further reduction of blood pressure is obtained.
Angina, Migraine and Essential Tremor
A starting dose of 40 mg two or three times daily may be increased by the same amount at weekly intervals according to patient response. An adequate response in migraine and essential tremor is usually seen in the range 80 to 160 mg/day and in angina in the range 120 to 240 mg/day.
Situational and Generalized Anxiety
A dose of 40 mg daily may provide short term relief of acute situational anxiety. Generalized anxiety, requiring longer term therapy, usually responds adequately to 40 mg twice daily which, in individual cases, may be increased to 40 mg three times daily. Treatment should be continued according to response. Patients should be reviewed after 6 to 12 months treatment.
Arrhythmias, Anxiety Tachycardia, Hypertrophic Obstructive Cardiomyopathy and Thyrotoxicosis
A dosage range of 10 to 40 mg three or four times a day usually achieves the required response.
Post Myocardial Infarction
Treatment should start between days 5 and 21 after myocardial infarction, with an initial dose of 40 mg four times a day for 2 or 3 days. In order to improve compliance the total daily dosage may thereafter be given as 80 mg twice a day.
Portal Hypertension
Dosage should be titrated to achieve approximately 25% reduction in resting heart rate. Dosage should begin with 40 mg twice daily, increasing to 80 mg twice daily depending on heart rate response. If necessary, the dose may be increased incrementally to a maximum of 160 mg twice daily.
Phaeochromocytoma
(Used only with an alpha-receptor blocking drug).
Pre-operative: 60 mg daily for 3 days is recommended. Non-operable malignant cases: 30 mg daily.
Elderly People
Evidence concerning the relation between blood level and age is conflicting. Propran should be used to treat the elderly with caution. It is suggested that treatment should start with the lowest dose. The optimum dose should be individually determined according to clinical response.
Pediatric Population
Dysrhythmias, Phaeochromocytoma, Thyrotoxicosis
Dosage should be individually determined and the following is only a guide: Oral: 0.25 to 0.5 mg/kg three or four times daily as required.
Migraine
Oral: Under the age of 12: 20 mg two or three times daily.
Over the age of 12: The adult dose.
Fallot's Tetralogy
The value of Propran in this condition is confined mainly to the relief of right-ventricular outflow tract shut-down. It is also useful for treatment of associated dysrhythmias and angina. Dosage should be individually determined and the following is only a guide:
Oral: Up to 1 mg/kg repeated three or four times daily as required.
METHOD OF ADMINISTRATION
For oral administration.
CONTRAINDICATIONS
SPECIAL WARNINGS AND PRECAUTIONS FOR USE
Propran as With other Beta-Blockers:
INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION
FERTILITY, PREGNANCY AND LACTATION
Pregnancy
As with all drugs Propran should not be given during pregnancy unless its use is essential. There is no evidence of teratogenicity with Propran. However beta-blockers reduce placental perfusion, which may result in intra-uterine fetal death, immature and premature deliveries. In addition, adverse effects (especially hypoglycemia and bradycardia in the neonate and bradycardia in the fetus) may occur. There is an increased risk of cardiac and pulmonary complications in the neonate in the post-natal period.
Breast-Feeding
Most beta-blockers, particularly lipophilic compounds, will pass into breast milk although to a variable extent. Breast-feeding is therefore not recommended following administration of these compounds.
Effects on Ability to Drive and Use Machines
Propran has no or negligible influence on the ability to drive and use machines. However it should be taken into account that occasionally dizziness or fatigue may occur.
UNDESIRABLE EFFECTS
Propran is usually well tolerated. In clinical studies the undesired events reported are usually attributable to the pharmacological actions of propranolol.
The following undesired events, listed by body system, have been reported. The following definitions of frequencies are used:
Very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to <1/1,000), very rare (<1/10,000), not known (cannot be estimated from the available data).
|
System Organ class |
Frequency |
Undesirable Effect |
|
Blood And Lymphatic System Disorders |
Rare |
Thrombocytopenia |
|
Endocrine Disorders |
Not known |
Hypoglycemia in neonates, infants, children, elderly patients, patients on hemodialysis, patients on concomitant antidiabetic therapy, patients with prolonged fasting and patients with chronic liver disease has been reported, seizure linked to hypoglycemia |
|
Nervous System Disorders |
Common |
Sleep disturbances, nightmares |
|
Rare |
Hallucinations, psychoses, mood changes, confusion, memory loss, paresthesia |
|
|
Very rare |
Isolated reports of myasthenia gravis like syndrome or exacerbation of myasthenia gravis have been reported |
|
|
Eye Disorders |
Rare |
Dry eyes, visual disturbances |
|
Cardiovascular Disorders |
Common |
Bradycardia, cold extremities, Raynaud's phenomenon |
|
Rare |
Heart failure deterioration, precipitation of heart block, postural hypotension, which may be associated with syncope, exacerbation of intermittent claudication |
|
|
Respiratory, Thoracic And Mediastinal Disorders |
Rare |
Bronchospasm may occur in patients with bronchial asthma or a history of asthmatic complaints, sometimes with fatal outcome |
|
Gastrointestinal Disorders |
Uncommon |
Gastrointestinal disturbance, such as nausea, vomiting, diarrhea |
|
Skin And Subcutaneous Tissue Disorders |
Rare |
Purpura, alopecia, psoriasiform skin reactions, exacerbation of psoriasis, skin rashes |
|
General Disorders And Administration Site Conditions |
Common |
Fatigue and/or lassitude (often transient) |
|
Rare |
Dizziness |
|
|
Investigations |
Very rare |
An increase in ANA (Antinuclear Antibodies) has been observed, however the clinical relevance of this is not clear |
Discontinuance of the drug should be considered if, according to clinical judgment, the well-being of the patient is adversely affected by any of the above reactions. Cessation of therapy with a beta-blocker should be gradual. In the rare event of intolerance, manifested as bradycardia and hypotension, the drug should be withdrawn and, if necessary, treatment for over dosage instituted.
Overdose
Propranolol is known to cause severe toxicity when used in overdose. Patients should be informed of the signs of overdose and advised to seek urgent medical assistance if an overdose of propranolol has been taken.
Clinical Features:
Cardiac
Bradycardia, hypotension, pulmonary edema, syncope and cardiogenic shock may develop. QRS complex prolongation, ventricular tachycardia, first to third degree AV block, ventricular fibrillation or asystole may also occur. Development of cardiovascular complications is more likely if other cardio active drugs, especially calcium channel blockers, digoxin, cyclic antidepressants or neuroleptics have also been ingested. Older patients and those with underlying ischemic heart disease are at risk of developing severe cardiovascular compromise.
CNS
Drowsiness, confusion, seizures, hallucinations, dilated pupils and in severe cases coma may occur. Neurological signs such as coma or absence of pupil reactivity are unreliable prognostic indicators during resuscitation.
Other Features
Bronchospasm, hyperkalaemia and occasionally CNS-mediated respiratory depression may occur.
Management
In cases of overdose or extreme falls in heart rate or blood pressure, treatment with propranolol must be stopped. Management should include general symptomatic and supportive measures including a clear airway and monitoring of vital signs until stable. In symptomatic patients, or patients with an abnormal ECG, early discussion with critical care should be considered.
Consult national clinical guidance for further information on the management of overdose.
PHARMACOLOGICAL PROPERTIES
Pharmacodynamic Properties
Pharmacotherapeutic Group: Beta Blocking Agents, Non-Selective
Propran is a competitive antagonist at both the beta1- and beta2 adrenoceptors. It has no agonist activity at the beta-adrenoceptor, but has membrane stabilizing activity at concentrations exceeding 1 to 3 mg/litre, though such concentrations are rarely achieved during oral therapy. Competitive beta-blockade has been demonstrated in man by a parallel shift to the right in the dose-heart rate response curve to beta agonists such as isoprenaline.
Propranolol as with other beta-blockers, has negative inotropic effects, and is therefore contraindicated in uncontrolled heart failure.
Propran is a racemic mixture and the active form is the S (-) isomer of propranolol. With the exception of inhibition of the conversion of thyroxin to triiodothyronine, it is unlikely that any additional ancillary properties possessed by R (+) propranolol, in comparison with the racemic mixture, will give rise to different therapeutic effects.
Propran is effective and well tolerated in most ethnic populations, although the response may be less in black patients.
Pharmacokinetic Properties
Following intravenous administration the plasma half-life of propranolol is about 2 hours and the ratio of metabolites to parent drug in the blood is lower than after oral administration. In particular 4-hydroxypropranolol is not present after intravenous administration. Propranolol is completely absorbed after oral administration and peak plasma concentrations occur 1 to 2 hours after dosing in fasting patients. The liver removes up to 90% of an oral dose with an elimination half-life of 3 to 6 hours. Propranolol is widely and rapidly distributed throughout the body with highest levels occurring in the lungs, liver, kidney, brain and heart. Propranolol is highly protein bound (80 to 95%).
Preclinical Safety Data
Propranolol is a drug on which extensive clinical experience has been obtained. Relevant information for the prescriber is provided elsewhere in this Summary of Product Characteristics.
Special Precautions for Storage
Store below 30°C. Store in the original package in order to protect from light and moisture.