

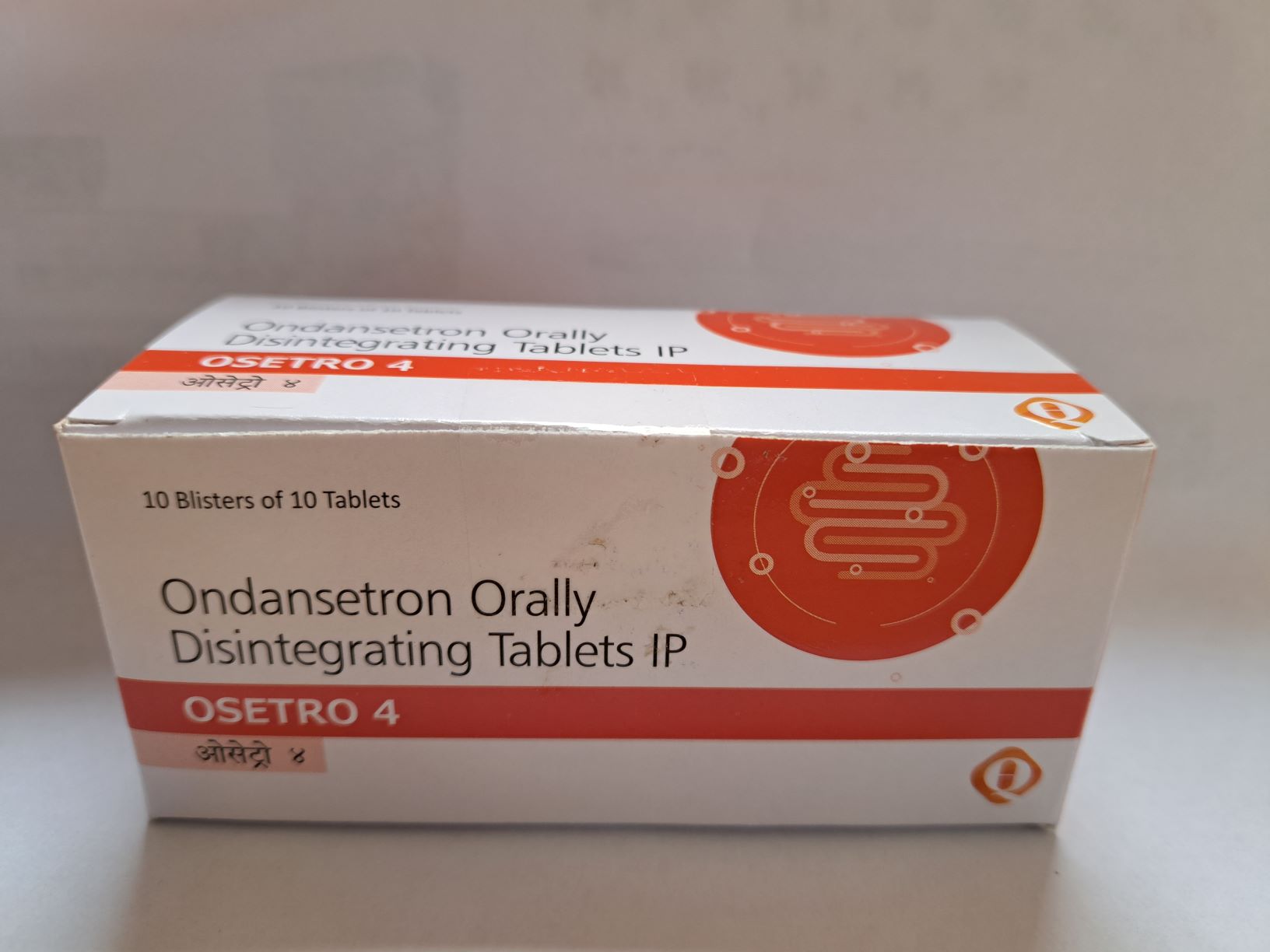
OSETRO 4 MG
Uncoated Orodispersible Tablet
Ondansetron (as hydrochloride) IP
Each Uncoated tablet OSETRO contains 4 mg Ondansetron (as Ondansetron hydrochloride). Antiemetic and antinauseants, Serotonin (5-HT3) antagonists. Chemotherapeutic agents and radiotherapy may cause release of 5-HT in the small intestine initiating a vomiting reflex by activating vagal afferents via 5-HT3 receptors.
PRESENTATION
Each Uncoated tablet contains 4 mg Ondansetron (as Ondansetron hydrochloride)
Packing: 10*10 Blister.
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics Properties
Pharmacotherapeutic Group: Antiemetic and antinauseants, Serotonin (5-HT3) antagonists
Mechanism of Action
Ondansetron is a potent, highly selective 5-HT3 receptor-antagonist. Its precise antiemetic and antinauseal mechanism of action is not known. Chemotherapeutic agents and radiotherapy may cause release of 5-HT in the small intestine initiating a vomiting reflex by activating vagal afferents via 5-HT3 receptors. Ondansetron blocks the initiation of this reflex. Activation of vagal afferents may also cause a release of 5-HT in the area postrema, located on the floor of the fourth ventricle, and this may also promote emesis through a central mechanism. Thus, the effect of ondansetron in the management of the nausea and vomiting induced by cytotoxic chemotherapy and radiotherapy is probably due to antagonism of 5-HT3 receptors on neurons located both in the peripheral and central nervous system. The mechanisms of action in post-operative nausea and vomiting are not known but there may be common pathways with cytotoxic induced nausea and vomiting.
In a pharmaco-psychological study in volunteers ondansetron has not shown a sedative effect. Ondansetron does not alter plasma prolactin concentrations. The role of ondansetron in opiate-induced emesis is not yet established.
Pediatrics Population:
Chemotherapy -Induced Nausea And Vomiting:
The efficacy of ondansetron in the control of emesis and nausea induced by cancer chemotherapy was assessed in a double-blind randomized trial in 415 patients aged 1 to 18 years. On the days of chemotherapy, patients received either ondansetron 5 mg/m2 i.v. + after 8-12 hrs. Ondansetron 4 mg p.o. or Ondansetron 0.45 mg/kg i.v. + after 8-12 hrs. Placebo p.o. Post-chemotherapy both groups received 4 mg ondansetron syrup twice daily for 3 days. Complete control of emesis on worst day of chemotherapy was 49% (5 mg/m2 i.v. + ondansetron 4 mg p.o.) and 41% (0.45 mg/kg i.v. + placebo p.o.). Post-chemotherapy both groups received 4 mg ondansetron syrup twice daily for 3 days.
A double-blind randomized placebo-controlled trial in 438 patients aged 1 to 17 years demonstrated complete control of emesis on worst day of chemotherapy in 73% of patients when ondansetron was administered intravenously at a dose of 5 mg/m2 i.v. together with 2-4 mg dexamethasone p.o. and in 71% of patients when ondansetron was administered as syrup at a dose of 8mg + 2- 4 mg dexamethasone p.o. on the days of chemotherapy. Post-chemotherapy both groups received 4 mg ondansetron syrup twice daily for 2 days.
The efficacy of ondansetron in 75 children aged 6 to 48 months was investigated in open-label, non-comparative, single-arm study. All children received three 0.15 mg/kg doses of intravenous ondansetron, administered at 30 minutes before the start of chemotherapy and then at four and eight hours after the first dose. Complete control of emesis was achieved in 56% of patients.
Another open-label, non-comparative, single-arm study investigated the efficacy of one intravenous dose of 0.15 mg/kg ondansetron followed by two oral ondansetron doses of 4mg for children aged < 12 yrs. and 8 mg for children aged ≥ 12 yrs. (total no. of children n= 28). Complete control of emesis was achieved in 42% of patients.
Prevention of Post-Operative Nausea and Vomiting:
The efficacy of a single dose of ondansetron in the prevention of post-operative nausea and vomiting was investigated in a randomized, double-blind, placebo-controlled study in 670 children aged 1 to 24 months (post-conceptual age ≥44 weeks, weight ≥ 3 kg). Included subjects were scheduled to undergo elective surgery under general anesthesia and had an ASA status ≤ III. A single dose of ondansetron 0.1 mg/kg was administered within five minutes following induction of anesthesia. The proportion of subjects who experienced at least one emetic episode during the 24-hour assessment period (ITT) was greater for patients on placebo than those receiving ondansetron ((28% vs. 11%, p <0.0001).
Four double-blind, placebo-controlled studies have been performed in 1469 male and female patients (2 to 12 years of age) undergoing general anesthesia. Patients were randomized to either single intravenous doses of ondansetron (0.1 mg/kg for pediatric patients weighing 40 kg or less, 4 mg for pediatric patients weighing more than 40 kg; number of patients = 735)) or placebo (number of patients = 734). Study drug was administered over at least 30 seconds, immediately prior to or following anesthesia induction. Ondansetron was significantly more effective than placebo in preventing nausea and vomiting. The results of these studies are summarized in Table 3.
Table Prevention and treatment of PONV in Pediatric Patients – Treatment response over 24 hours
|
Study |
Endpoint |
Ondansetron % |
Placebo % |
p value |
|
S3A380 |
CR |
68 |
39 |
≤0.001 |
|
S3GT09 |
CR |
61 |
35 |
≤0.001 |
|
S3A381 |
CR |
53 |
17 |
≤0.001 |
|
S3GT11 |
no nausea |
64 |
51 |
0.004 |
|
S3GT11 |
no emesis |
60 |
47 |
0.004 |
CR = no emetic episodes, rescue or withdrawal
Pharmacokinetic Properties
Absorption
Following oral administration of ondansetron, absorption is rapid with maximum peak plasma concentrations of about 30ng/mL being attained and achieved in approximately 1.5 hours after an 8mg dose.
Distribution
The syrup and tablet formulations are bioequivalent and have an absolute oral bioavailability of 60%.
Elimination
The disposition of ondansetron following oral, intravenous and intramuscular dosing is similar with a terminal elimination half-life of approximately 3 hours and a steady- state volume of distribution of about 140L. Ondansetron is not highly protein bound (70-76%) and is cleared from the systemic circulation predominantly by hepatic metabolism through multiple enzymatic pathways. Less than 5% of the absorbed dose is excreted unchanged in the urine. The absence of the enzyme CYP2D6 (the debrisoquine polymorphism) has no effect on the pharmacokinetics of ondansetron. The pharmacokinetic properties of ondansetron are unchanged on repeat dosing.
The protein binding of ondansetron is 70-76%. A direct effect of plasma concentration and anti-emetic effect has not been established. Ondansetron is cleared from the systemic circulation predominantly by hepatic metabolism through multiple enzymatic pathways. Less than 5% of the absorbed dose is excreted unchanged in the urine. The absence of the enzyme CYP2D6 has no effect on ondansetron's pharmacokinetics. The pharmacokinetic properties of ondansetron are unchanged on repeat dosing.
In a study of 21 pediatric patients aged between 3 and 12 years undergoing elective surgery with general anesthesia, the absolute values for both the clearance and volume of distribution of ondansetron following a single intravenous dose of 2mg (3-7 years old) or 4mg (8-12 years old) were reduced. The magnitude of the change was age-related, with clearance falling from about 300mL/min at 12 years of age to 100mL/min at 3 years. Volume of distribution fell from about 75L at 12 years to 17L at 3 years. Use of weight-based dosing (0.1mg/kg up to 4mg maximum) compensates for these changes and is effective in normalizing systemic exposure in pediatrics patients.
In patients with renal impairment (creatinine clearance 15-60 ml/min), both systemic clearance and volume of distribution are reduced following IV administration of ondansetron, resulting in a slight, but clinically insignificant, increase in elimination half-life (5.4h). A study in patients with severe renal impairment who required regular hemodialysis (studied between dialyses) showed Ondansetron's pharmacokinetics to be essentially unchanged following IV administration.
Following oral, intravenous or intramuscular dosing in patients with severe hepatic impairment, ondansetron's systemic clearance is markedly reduced with prolonged elimination half-lives (15-32 h) and an oral bioavailability approaching 100% due to reduced pre-systemic metabolism.
Special Patient Populations
Children and Adolescents (Aged 1 Month to 17 Years)
In pediatrics patients aged 1 to 4 months (n=19) undergoing surgery, weight normalized clearance was approximately 30% slower than in patients aged 5 to 24 months (n=22) but comparable to the patients aged 3 to 12 years. The half-life in the patient population aged 1 to 4 month was reported to average 6.7 hours compared to 2.9 hours for patients in the 5 to 24 month and 3 to 12 year age range. The differences in pharmacokinetic parameters in the 1 to 4 month patient population can be explained in part by the higher percentage of total body water in neonates and infants and a higher volume of distribution for water soluble drugs like ondansetron.
In pediatric patients aged 3 to 12 years undergoing elective surgery with general anesthesia, the absolute values for both the clearance and volume of distribution of ondansetron were reduced in comparison to values with adult patients. Both parameters increased in a linear fashion with weight and by 12 years of age, the values were approaching those of young adults. When clearance and volume of distribution values were normalized by body weight, the values for these parameters were similar between the different age group populations. Use of weight-based dosing compensates for age-related changes and is effective in normalizing systemic exposure in pediatrics patients.
Population pharmacokinetic analysis was performed on 74 pediatric cancer patients aged 6 to 48 months and 41 surgery patients aged 1 to 24 months following intravenous administration of ondansetron. Based on the population pharmacokinetic parameters for patients aged 1 month to 48 months, administration of the adult weight based dose (0.15 mg/kg intravenously every 4 hours for 3 doses) would result in a systemic exposure (AUC) comparable to that observed in pediatric surgery patients (aged 5 to 24 months), pediatrics cancer patients (aged 4 to 18 years), and surgical patients (aged 3 to 12 years), at similar doses, as shown in Table C. This exposure (AUC) is consistent with the exposure-efficacy relationship described previously in pediatrics cancer subjects, which showed a 50% to 90% response rate with AUC values ranging from 170 to 250 ng.h/ml.
Table. Pharmacokinetics in pediatric Patients 1 Month to 18 Years of Age
|
Study |
Patient population (Intravenous dose) |
Age |
N |
AUC (ng.h/mL) |
CL (L/h/kg) |
Vdss (L/kg) |
T1/2 (h) |
|
Geometric mean |
Mean |
||||||
|
S3A403191 |
Surgery (0.1 or 0.2mg/kg) |
1 to 4 months |
19 |
360 |
0.401 |
3.5 |
6.7 |
|
S3A403191 |
Surgery (0.1 or 0.2mg/kg) |
5 to 24 months |
22 |
236 |
0.581 |
2.3 |
2.9 |
|
S3A40320 & S3A40319 Pop PK2&3 |
Cancer/Surgery (0.15mg/kg q4h/ 0.1 or 0.2mg/kg) |
1 to 48 months |
115 |
257 |
0.582 |
3.65 |
4.9 |
|
S3KG024 |
Surgery (2mg or 4mg) |
3 to 12 years |
21 |
240 |
0.439 |
1.65 |
2.9 |
|
S3A-150 |
Cancer (0.15mg/kg q4h) |
4 to 18 years |
21 |
247 |
0.599 |
1.9 |
2.8 |
1 Ondansetron single intravenous dose: 0.1 or 0.2 mg/kg
2 Population PK patients: 64% cancer patients and 36% surgery patients.
3 Population estimates shown; AUC based on dose of 0.15 mg/kg.
4 Ondansetron single intravenous dose: 2 mg (3 to 7 years) or 4 mg (8 to 12 years)
INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION
Based on reports of profound hypotension and loss of consciousness when ondansetron was administered with Apo morphine hydrochloride, concomitant use with Apo morphine is contraindicated.
Use of ondansetron with QT prolonging drugs may result in additional QT prolongation. Concomitant use of ondansetron with cardio toxic drugs (e.g. anthracyclines such as doxorubicin, daunorubicin or trastuzimab), antibiotics (such as erythromycin or ketoconazole), antiarrhythmic (such as amiodarone) and beta blockers (such as atenolol or timolol) may increase the risk of arrhythmias. (See Special warnings and precautions for use).
CLINICAL PARTICULARS
Therapeutic Indications
Adults:
Ondansetron is indicated for the management of nausea and vomiting induced by cytotoxic chemotherapy and radiotherapy, and for the prevention and treatment of post-operative nausea and vomiting (PONV).
Pediatrics population:
Ondansetron is indicated for the management of chemotherapy-induced nausea and vomiting (CINV) in children aged ≥ 6 months, and for the prevention and treatment of PONV in children aged ≥ 1 month.
POSOLOGY AND METHOD OF ADMINISTRATION
Posology
Oral use. Place the Orodispersible tablet on top of the tongue, where it will disperse within seconds, then swallow.
Chemotherapy and Radiotherapy induced nausea and vomiting:
Adults:
The emetogenic potential of cancer treatment varies according to the doses and combinations of chemotherapy and radiotherapy regimens used. The route of administration and dose of ondansetron should be flexible in the range of 8-32 mg a day and selected as shown below.
Emetogenic Chemotherapy and Radiotherapy:
For oral administration: 8 mg 1-2 hours before treatment, followed by 8 mg 12 hours later. To protect against delayed or prolonged emesis after the first 24 hours, oral or rectal treatment with ondansetron should be continued for up to 5 days after a course of treatment. The recommended dose for oral administration is 8 mg twice daily.
Highly Emetogenic Chemotherapy
For patients receiving highly emetogenic chemotherapy, e.g. high-dose cisplatin, ondansetron can be given by intravenous administration.
To protect against delayed or prolonged emesis after the first 24 hours, oral treatment with ondansetron should be continued for up to 5 days after a course of treatment. The recommended dose for oral administration is 8 mg twice daily.
Pediatric Population:
Chemotherapy induced nausea and vomiting in children aged ≥6 months and adolescents. The dose for chemotherapy-induced nausea and vomiting can be calculated based on body surface area (BSA) or weight – see below. Weight-based dosing results in higher total daily doses compared to BSA-based dosing. There are no data from controlled clinical trials on the use of ondansetron in the prevention of chemotherapy-induced delayed or prolonged nausea and vomiting. There are no data from controlled clinical trials on the use of ondansetron for radiotherapy-induced nausea and vomiting in children.
Dosing by BSA:
Ondansetron should be administered immediately before chemotherapy as a single intravenous dose of 5 mg/m2. The intravenous dose must not exceed 8mg. Oral dosing can commence twelve hours later and may be continued for up to 5 days. See table 1 below. The total daily dose must not exceed adult dose of 32 mg.
Table 1: BSA-based dosing for chemotherapy – Children aged ≥6 months and adolescents
|
BSA |
Day1a,b |
Days 2-6b |
|
< 0.6m2 |
5 mg/m2 i.v. 2mg syrup or tablet after 12 hours |
2 mg syrup or tablet every 12 hours |
|
> 0.6 m2 |
5 mg/m2 i.v. 4mg syrup or tablet after 12 hours |
4 mg syrup or tablet every 12 hours |
a: The intravenous dose must not exceed 8mg.
b: The total daily dose must not exceed adult dose of 32mg.
Dosing By Body Weight:
Weight-based dosing results in higher total daily doses compared to BSA-based dosing. Ondansetron should be administered immediately before chemotherapy as a single intravenous dose of 0.15 mg/kg. The intravenous dose must not exceed 8mg.
Two further intravenous doses may be given in 4-hourly intervals. The total daily dose must not exceed adult dose of 32 mg. Oral dosing can commence twelve hours later and may be continued for up to 5 days. See table 2 below.
Table2: Weight-based dosing for chemotherapy – children aged ≥6 months and adolescents
|
Weight |
Day 1a,b |
Days 2-6b |
|
≤ 10kg |
Up to 3 doses of 0.15mg/kg at 4-hourly intervals. |
2 mg syrup or tablet every 12 hours |
|
> 10kg |
Up to 3 doses of 0.15mg/kg at 4-hourly intervals. |
4 mg syrup or tablet every 12 hours |
a: The intravenous dose must not exceed 8mg.
b: The total daily dose must not exceed adult dose of 32 mg.
Elderly
Ondansetron is well tolerated by patients over 65 years and no alteration of dosage, dosing frequency or route of administration are required.
Post-operative nausea and vomiting (PONV):
Adults
For the prevention of PONV ondansetron may be administered orally or by intravenous injection.
For Oral Administration:
16 mg one hour prior to anesthesia. Alternatively, 8 mg one hour prior to anesthesia followed by two further doses of 8 mg at eight hourly intervals.
Treatment of Established PONV
For the treatment of established PONV intravenous administration is recommended.
Pediatric Population:
Post-operative nausea and vomiting in children aged ≥ 1 months and adolescents:
Oral Formulations:
No studies have been conducted on the use of orally administered ondansetron in the prevention or treatment of post-operative nausea and vomiting, slow i.v. injection is recommended for this purpose.
Injection:
For prevention of PONV in pediatric patients having surgery performed under general anesthesia, a single dose of ondansetron may be administered by slow intravenous injection (not less than 30 seconds) at a dose of 0.1 mg/kg up to a maximum of 4mg either prior to, at or after induction of anesthesia.
For the treatment of PONV after surgery in pediatrics patients having surgery performed under general anesthesia, a single dose of ondansetron may be administered by slow intravenous injection (not less than 30 seconds) at a dose of 0.1 mg/kg up to a maximum of 4 mg.
There are no data on the use of ondansetron for the treatment of post-operative vomiting in children under 2 years of age.
Elderly
There is limited experience in the use of ondansetron in the prevention and treatment of post-operative nausea and vomiting (PONV) in the elderly, however ondansetron is well tolerated in patients over 65 years receiving chemotherapy.
Special Populations:
Patients with Renal Impairment
No alteration of daily dosage or frequency of dosing, or route of administration is required.
Patients with Hepatic Impairment
Clearance of ondansetron is significantly reduced and serum half-life significantly prolonged in subjects with moderate or severe impairment of hepatic function. In such patients a total daily dose of 8 mg should not be exceeded.
Patients with Poor Sparteine/Debrisoquine Metabolism
The elimination half-life of ondansetron is not altered in subjects classified as poor metabolizers of sparteine and debrisoquine. Consequently in such patients, repeat dosing will give medicinal product exposure levels no different from those of the general population. No alteration of daily dosage or frequency of dosing are required.
Adverse events are listed below by system organ class and frequency. Frequencies are defined as:
Very common (≥1/10)
Common (≥1/100 to <1/10)
Uncommon (≥1/1,000 to <1/100)
Rare (≥1/10,000 to <1/1,000)
Very rare (<1/10,000) not known (cannot be estimated from the available data)
Very common, common and uncommon events were generally determined from clinical trial data. The incidence in placebo was taken into account. Rare and very rare events were generally determined from post-marketing spontaneous data.
Very rarely transient ECG changes including QT interval prolongation have been reported
The following frequencies are estimated at the standard recommended doses of ondansetron according to indication and formulation.
Rare: Immediate hypersensitivity reactions sometimes severe, including anaphylaxis.
There may be cross-sensitivity with other selective 5-HT3- antagonists.
Very common: Headache.
Uncommon: Extrapyramidal reactions (such as oculogyric crisis, dystonic reactions and dyskinesia) have been observed without definitive evidence of persistent clinical sequelae; seizures.
Rare: Dizziness during rapid IV administration.
Rare: Transient visual disturbances (e.g. blurred vision) predominantly during rapid intravenous administration.
Very Rare: Transient blindness predominantly during intravenous administration.
The majority of the blindness cases reported resolved within 20 minutes. Most patients had received chemotherapeutic agents, which included cisplatin. Some cases of transient blindness were reported as cortical in origin.
Uncommon: Arrhythmias, chest pain with or without ST segment depression, bradycardia.
Rare: QTc prolongation (including Torsade de pointes)
Common: Sensation of warmth or flushing.
Uncommon: Hypotension.
Uncommon: Hiccups.
Common: Ondansetron is known to increase the large bowel transit time and may cause constipation in some patients. Local burning sensation following insertion of suppositories.
Uncommon: Asymptomatic increases in liver function tests.
These events were observed commonly in patients receiving chemotherapy with cisplatin.
General Disorders and Administration Site Conditions
Common: Local IV injection site reactions.
Pediatrics population
The adverse event profile in children and adolescents was comparable to that seen in adults.
OVERDOSE
Little is known at present about over dosage with ondansetron, however, a limited number of patients received overdoses. In the majority of cases symptoms were similar to those already reported in patients receiving recommended doses (see section Undesirable Effects). Manifestations that have been reported include visual disturbances, severe constipation, hypotension and a vasovagal episode with transient second-degree AV block.
Ondansetron prolongs QT interval in a dose-dependent manner. ECG monitoring is recommended in cases of overdose.
Treatment
There is no specific antidote for ondansetron, therefore in all cases of suspected overdose, symptomatic and supportive therapy should be given as appropriate. The use of ipecacuanha to treat overdose with Ondansetron is not recommended, as patients are unlikely to respond due to the anti-emetic action of Ondansetron itself.
Pediatrics population
Pediatrics cases consistent with serotonin syndrome have been reported after inadvertent oral overdoses of ondansetron (exceeded estimated ingestion of 4 mg/kg) in infants and children aged 12 months to 2 years.
SPECIAL WARNINGS AND PRECAUTIONS FOR USE
Pediatric Population:
Chemotherapy-Induced Nausea and Vomiting:
FERTILITY, PREGNANCY AND LACTATION
Women of childbearing potential should consider the use of contraception.
Based on human experience from epidemiological studies, ondansetron is suspected to cause Oro facial malformations when administered during the first trimester of pregnancy.
In one cohort study including 1.8 million pregnancies, first trimester ondansetron use was associated with an increased risk of oral clefts (3 additional cases per 10 000 women treated; adjusted relative risk, 1.24, (95% CI 1.03-1.48)).
The available epidemiological studies on cardiac malformations show conflicting results. Animal studies do not indicate direct or indirect harmful effects with respect to reproductive toxicity.
Ondansetron should not be used during the first trimester of pregnancy.
Tests have shown that ondansetron passes into the milk of lactating animals. It is therefore recommended that mothers receiving ondansetron should not breast-feed their babies.
In psychomotor testing ondansetron does not impair performance nor cause sedation. No detrimental effects on such activities are predicted from the pharmacology of ondansetron.
CONTRAINDICATIONS