

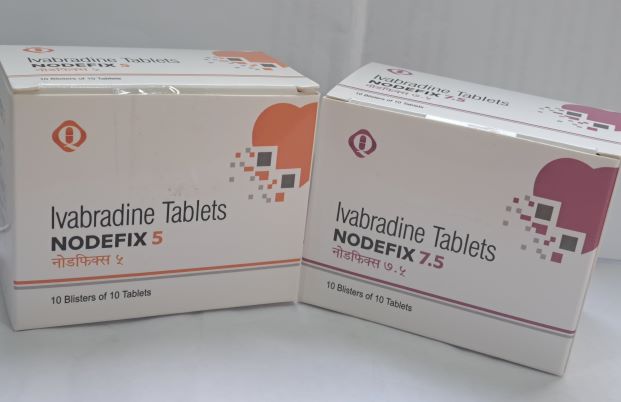
NODEFIX
Ivabradine HCL
PRESENTATION:
Each Film Coated Tablet Contains Ivabradine HCL 5 & 7.5 mg.
Pack Size: 10*10
Packing: Blister
CLINICAL PARTICULARS
Therapeutic Indications
Symptomatic treatment of chronic stable angina pectoris Ivabradine is indicated for the symptomatic treatment of chronic stable angina pectoris in coronary artery disease adults with normal sinus rhythm and heart rate ≥ 70 bpm Ivabradine is indicated:
In adults unable to tolerate or with a contraindication to the use of beta-blockers.
Or in combination with beta-blockers in patients inadequately controlled with an optimal beta- blocker dose.
Treatment of Chronic Heart Failure Ivabradine is indicated in chronic heart failure NYHA II to IV class with systolic dysfunction, in patients in sinus rhythm and whose heart rate is ≥ 75 bpm, in combination with standard therapy including beta-blocker therapy or when beta-blocker therapy is contraindicated or not tolerated.
Posology and Method of Administration
Posology
For the different doses, film-coated tablets containing 5 mg and 7.5 mg ivabradine are available. Symptomatic treatment of chronic stable angina pectoris
It is recommended that the decision to initiate or titrate treatment takes place with the availability of serial heart rate measurements, ECG or ambulatory 24-hour monitoring.
The starting dose of ivabradine should not exceed 5 mg twice daily in patients aged below 75 years. After three to four weeks of treatment, if the patient is still symptomatic, if the initial dose is well tolerated and if resting heart rate remains above 60 bpm, the dose may be increased to the next higher dose in patients receiving 2.5 mg twice daily or 5 mg twice daily. The maintenance dose should not exceed 7.5 mg twice daily.
If there is no improvement in symptoms of angina within 3 months after start of treatment, treatment of ivabradine should be discontinued.
In addition, discontinuation of treatment should be considered if there is only limited symptomatic response and when there is no clinically relevant reduction in resting heart rate within three months.
If, during treatment, heart rate decreases below 50 beats per minute (bpm) at rest or the patient experiences symptoms related to bradycardia such as dizziness, fatigue or hypotension, the dose must be titrated downward including the lowest dose of 2.5 mg twice daily (one half 5 mg tablet twice daily). After dose reduction, heart rate should be monitored. Treatment must be discontinued if heart rate remains below 50 bpm or symptoms of bradycardia persist despite dose reduction.
Treatment of Chronic Heart Failure The treatment has to be initiated only in patient with stable heart failure. It is recommended that the treating physician should be experienced in the management of chronic heart failure. The usual recommended starting dose of ivabradine is 5 mg twice daily. After two weeks of treatment, the dose can be increased to 7.5 mg twice daily if resting heart rate is persistently above 60 bpm or decreased to 2.5 mg twice daily (one half 5 mg tablet twice daily) if resting heart rate is persistently below 50 bpm or in case of symptoms related to bradycardia such as dizziness, fatigue or hypotension. If heart rate is between 50 and 60 bpm, the dose of 5 mg twice daily should be maintained.
If during treatment, heart rate decreases persistently below 50 beats per minute (bpm) at rest or the patient experiences symptoms related to bradycardia, the dose must be titrated downward to the next lower dose in patients receiving 7.5 mg twice daily or 5 mg twice daily. If heart rate increases persistently above 60 beats per minute at rest, the dose can be up titrated to the next upper dose in patients receiving 2.5 mg twice daily or 5 mg twice daily.
Treatment must be discontinued if heart rate remains below 50 bpm or symptoms of bradycardia persist.
Special Population
Elderly
In patients aged 75 years or more, a lower starting dose should be considered (2.5 mg twice daily i.e. one half 5 mg tablet twice daily) before up-titration if necessary.
Renal impairment
No dose adjustment is required in patients with renal insufficiency and creatinine clearance above 15 ml/min. No data are available in patients with creatinine clearance below 15 ml/min. Ivabradine should therefore be used with precaution in this population.
Hepatic Impairment
No dose adjustment is required in patients with mild hepatic impairment. Caution should be exercised when using ivabradine in patients with moderate hepatic impairment.
Ivabradine is contraindicated for use in patients with severe hepatic insufficiency, since it has not been studied in this population and a large increase in systemic exposure is anticipated.
Pediatric Population
The safety and efficacy of ivabradine for the treatment of chronic heart failure in children aged below 18 years have not been established.
Method of Administration
Tablets must be taken orally twice daily, i.e. once in the morning and once in the evening during meals.
CONTRAINDICATIONS
Hypersensitivity to the active substance or to any of the excipients
Resting heart rate below 70 beats per minute prior to treatment
Cardiogenic shock
Acute myocardial infarction
Severe hypotension (< 90/50 mmHg) Severe hepatic insufficiency
Sick sinus syndrome
Sino-atrial block
Unstable or acute heart failure
Pacemaker dependent (heart rate imposed exclusively by the pacemaker)
Unstable angina
AV-block of 3rd degree
Combination with strong cytochrome P450 3A4 inhibitors such as azole antifungals (ketoconazole, itraconazole), macrolide antibiotics (clarithromycin, erythromycin per os, josamycin, telithromycin), HIV protease inhibitors (nelfinavir, ritonavir) and nefazodone Combination with verapamil or diltiazem which are moderate CYP3A4 inhibitors with heart rate reducing properties
Pregnancy, lactation and women of child-bearing potential not using appropriate contraceptive measures
SPECIAL WARNINGS AND PRECAUTIONS FOR USE
Special Warnings
Lack of benefit on clinical outcomes in patients with symptomatic chronic stable angina pectoris Ivabradine is indicated only for symptomatic treatment of chronic stable angina pectoris because ivabradine has no benefits on cardiovascular outcomes (e.g. myocardial infarction or cardiovascular death).
Measurement of Heart Rate
Given that the heart rate may fluctuate considerably over time, serial heart rate measurements, ECG or ambulatory 24-hour monitoring should be considered when determining resting heart rate before initiation of ivabradine treatment and in patients on treatment with ivabradine when titration is considered. This also applies to patients with a low heart rate, in particular when heart rate decreases below 50 bpm, or after dose reduction.
Cardiac Arrhythmias
Ivabradine is not effective in the treatment or prevention of cardiac arrhythmias and likely loses its efficacy when a tachyarrhythmia occurs (e.g. ventricular or supraventricular tachycardia).
Ivabradine is therefore not recommended in patients with atrial fibrillation or other cardiac arrhythmias that interfere with sinus node function. In patients treated with ivabradine the risk of developing atrial fibrillation is increased. Atrial fibrillation has been more common in patients using concomitantly amiodarone or potent class I anti-arrhythmic. It is recommended to regularly clinically monitor ivabradine treated patients for the occurrence of atrial fibrillation (sustained or paroxysmal), which should also include ECG monitoring if clinically indicated (e.g. in case of exacerbated angina, palpitations, irregular pulse).
Patients should be informed of signs and symptoms of atrial fibrillation and be advised to contact their physician if these occur.
If atrial fibrillation develops during treatment, the balance of benefits and risks of continued ivabradine treatment should be carefully reconsidered.
Chronic heart failure patients with intraventricular conduction defects (bundle branch block left, bundle branch block right) and ventricular dyssynchrony should be monitored closely.
Use in Patients with AV-Block of 2nd Degree
Ivabradine is not recommended in patients with AV-block of 2nd degree.
Use in Patients with a Low Heart Rate
Ivabradine must not be initiated in patients with a pre-treatment resting heart rate below 70 beats per minute. If, during treatment, resting heart rate decreases persistently below 50 bpm or the patient experiences symptoms related to bradycardia such as dizziness, fatigue or hypotension, the dose must be titrated downward or treatment discontinued if heart rate below 50 bpm or symptoms of bradycardia persist.
Combination with Calcium Channel Blockers
Concomitant use of ivabradine with heart rate reducing calcium channel blockers such as verapamil or diltiazem is contraindicated. No safety issue has been raised on the combination of ivabradine with nitrates and dihydropyridine calcium channel blockers such as amlodipine. Additional efficacy of ivabradine in combination with dihydropyridine calcium channel blockers has not been established.
Chronic Heart Failure
Heart failure must be stable before considering ivabradine treatment. Ivabradine should be used with caution in heart failure patients with NYHA functional classification IV due to limited amount of data in this population. Stroke The use of ivabradine is not recommended immediately after a stroke since no data is available in these situations. Visual Function
Ivabradine influences on retinal function. There is no evidence of a toxic effect of long-term ivabradine treatment on the retina. Cessation of treatment should be considered if any unexpected deterioration in visual function occurs. Caution should be exercised in patients with retinitis pigmentosa.
PRECAUTIONS FOR USE
Patients with Hypotension Limited data are available in patients with mild to moderate hypotension, and ivabradine should therefore be used with caution in these patients. Ivabradine is contra-indicated in patients with severe hypotension (blood pressure < 90/50 mmHg).
Atrial Fibrillation - Cardiac Arrhythmias There is no evidence of risk of (excessive) bradycardia on return to sinus rhythm when pharmacological cardio version is initiated in patients treated with ivabradine. However, in the absence of extensive data, non-urgent DC-cardio version should be considered 24 hours after the last dose of ivabradine.
Use in Patients with Congenital QT Syndrome or Treated With QT Prolonging Medicinal Products
The use of ivabradine in patients with congenital QT syndrome or treated with QT prolonging medicinal products should be avoided. If the combination appears necessary, close cardiac monitoring is needed. Heart rate reduction, as caused by ivabradine, may exacerbate QT prolongation, which may give rise to severe arrhythmias, in particular Torsade de pointes.
Hypertensive Patients Requiring Blood Pressure Treatment Modifications. In the SHIFT trial more patients experienced episodes of increased blood pressure while treated with ivabradine (7.1%) compared to patients treated with placebo (6.1%). These episodes occurred most frequently shortly after blood pressure treatment was modified, were transient, and did not affect the treatment effect of ivabradine. When treatment modifications are made in chronic heart failure patients treated with ivabradine blood pressure should be monitored at an appropriate interval.
INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION
Pharmacodynamics Interactions Concomitant Use Not Recommended QT Prolonging Medicinal Products o Cardiovascular QT prolonging medicinal products (e.g. quinidine, disopyramide, bepridil, sotalol, ibutilide, amiodarone).
o Non-cardiovascular QT prolonging medicinal products (e.g. pimozide, ziprasidone, sertindole, mefloquine, halofantrine, pentamidine, cisapride, intravenous erythromycin).
The concomitant use of cardiovascular and non-cardiovascular QT prolonging medicinal products with ivabradine should be avoided since QT prolongation may be exacerbated by heart rate reduction. If the combination appears necessary, close cardiac monitoring is needed.
Concomitant Use with Precaution Potassium-depleting diuretics (thiazide diuretics and loop diuretics): hypokalemia can increase the risk of arrhythmia. As ivabradine may cause bradycardia, the resulting combination of hypokalemia and bradycardia is a predisposing factor to the onset of severe arrhythmias, especially in patients with long QT syndrome, whether congenital or substance-induced. Pharmacokinetic interactions
Cytochrome P450 3A4 (CYP3A4) Ivabradine is metabolized by CYP3A4 only and it is a very weak inhibitor of this cytochrome. Ivabradine was shown not to influence the metabolism and plasma concentrations of other CYP3A4 substrates (mild, moderate and strong inhibitors). CYP3A4 inhibitors and inducers are liable to interact with ivabradine and influence its metabolism and pharmacokinetics to a clinically significant extent. Drug-drug interaction studies have established that CYP3A4 inhibitors increase ivabradine plasma concentrations, while inducers decrease them. Increased plasma concentrations of ivabradine may be associated with the risk of excessive bradycardia.
Contraindication of Concomitant Use The concomitant use of potent CYP3A4 inhibitors such as azole antifungals (ketoconazole, itraconazole), macrolide antibiotics (clarithromycin, erythromycin per os, josamycin, and telithromycin), HIV protease inhibitors (nelfinavir, ritonavir) and nefazodone is contraindicated (see section 4.3). The potent CYP3A4 inhibitors ketoconazole (200 mg once daily) and josamycin (1 g twice daily) increased ivabradine mean plasma exposure by 7 to 8 fold. Moderate CYP3A4 inhibitors: specific interaction studies in healthy volunteers and patients have shown that the combination of ivabradine with the heart rate reducing agents diltiazem or verapamil resulted in an increase in ivabradine exposure (2 to 3 fold increase in AUC) and an additional heart rate reduction of 5 bpm. The concomitant use of ivabradine with these medicinal products is contraindicated.
Concomitant Use Not Recommended Grapefruit juice: ivabradine exposure was increased by 2-fold following the co-administration with grapefruit juice. Therefore the intake of grapefruit juice should be avoided.
Concomitant Use with Precautions o Moderate CYP3A4 inhibitors: the concomitant use of ivabradine with other moderate CYP3A4 inhibitors (e.g. fluconazole) may be considered at the starting dose of 2.5 mg twice daily and if resting heart rate is above 70 bpm, with monitoring of heart rate.
o CYP3A4 inducers: CYP3A4 inducers (e.g. rifampicin, barbiturates, phenytoin, Hypericum perforatum [St John's Wort]) may decrease ivabradine exposure and activity. The concomitant use of CYP3A4 inducing medicinal products may require an adjustment of the dose of ivabradine. The combination of ivabradine 10 mg twice daily with St John's Wort was shown to reduce ivabradine AUC by half. The intake of St John's Wort should be restricted during the treatment with ivabradine.
Other Concomitant Use Specific drug-drug interaction studies have shown no clinically significant effect of the following medicinal products on pharmacokinetics and pharmacodynamics of ivabradine: proton pump inhibitors (omeprazole, lansoprazole), sildenafil, HMG CoA reductase inhibitors (simvastatin), dihydropyridine calcium channel blockers (amlodipine, lacidipine), digoxin and warfarin. In addition there was no clinically significant effect of ivabradine on the pharmacokinetics of simvastatin, amlodipine, lacidipine, on the pharmacokinetics and pharmacodynamics of digoxin, warfarin and on the pharmacodynamics of aspirin. In pivotal phase III clinical trials the following medicinal products were routinely combined with ivabradine with no evidence of safety concerns: angiotensin converting enzyme inhibitors, angiotensin II antagonists, beta-blockers, diuretics, anti-aldosterone agents, short and long acting nitrates, HMG CoA reductase inhibitors, fibrates, proton pump inhibitors, oral antidiabetics, aspirin and other anti- platelet medicinal products.
Pediatric Population Interaction studies have only been performed in adults.
FERTILITY, PREGNANCY AND LACTATION
Women of childbearing potential Women of child-bearing potential should use appropriate contraceptive measures during treatment.
Pregnancy
There are no or limited amount of data from the use of ivabradine in pregnant women. Studies in animals have shown reproductive toxicity. These studies have shown embryo toxic and teratogenic effects. The potential risk for humans is unknown. Therefore, ivabradine is contraindicated during pregnancy.
Breastfeeding
Animal studies indicate that ivabradine is excreted in milk. Therefore, ivabradine is contraindicated during breast-feeding. Women that need treatment with ivabradine should stop breast-feeding, and choose for another way of feeding their child.
Fertility
Studies in rats have shown no effect on fertility in males and females.
Effects on Ability to Drive and Use Machines A specific study to assess the possible influence of ivabradine on driving performance has been performed in healthy volunteers where no alteration of the driving performance was evidenced. However, in post-marketing experience, cases of impaired driving ability due to visual symptoms have been reported. Ivabradine may cause transient luminous phenomena consisting mainly of phosphenes (see section 4.8). The possible occurrence of such luminous phenomena should be taken into account when driving or using machines in situations where sudden variations in light intensity may occur, especially when driving at night. Ivabradine has no influence on the ability to use machines.
UNDESIRABLE EFFECTS
Summary of the Safety Profile Ivabradine has been studied in clinical trials involving nearly 45,000 participants. The most common adverse reactions with ivabradine, luminous phenomena (phosphenes) and bradycardia, are dose dependent and related to the pharmacological effect of the medicinal product.
Tabulated List of Adverse Reactions
The following adverse reactions have been reported during clinical trials and are ranked using the following frequency: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); very rare (<1/10,000); not known (cannot be estimated from the available data).
Blood and Lymphatic System Disorders
Uncommon Eosinophilia
Metabolism and nutrition disorders
Uncommon Hyperuricaemia
Nervous System Disorders
Common Headache, generally during the first month of treatment Dizziness,
possibly related to bradycardia
Uncommon* Syncope, possibly related to bradycardia
Eye Disorders
Very Common Luminous phenomena (phosphenes)
Common Blurred vision Uncommon* Diplopia Visual impairment Ear and labyrinth disorders
Uncommon Vertigo Cardiac disorders Common Bradycardia AV1st degree block (ECG prolonged PQ interval) Ventricular extra systoles Atrial fibrillation
Uncommon Palpitations, supraventricular extra systoles
Very Rare AV 2nd degree block, AV 3rd degree block Sick sinus syndrome
Vascular disorders
Common Uncontrolled blood pressure
Uncommon* Hypotension, possibly related to bradycardia
Respiratory, thoracic and mediastina disorders
Uncommon Dyspnea
Gastrointestinal Disorders
Uncommon Nausea Constipation Diarrhea Abdominal pain* Skin and subcutaneous tissue disorders
Uncommon* Angioedema Rash Rare* Erythema Pruritus Urticaria
Musculoskeletal and Connective Tissue Disorders
Uncommon Muscle spasms
General Disorders and Administration Site Conditions
Uncommon* Asthenia, possibly related to bradycardia Fatigue, possibly related to bradycardia
Rare* Malaise, possibly related to bradycardia
Investigations
Uncommon Elevated creatinine in blood ECG prolonged QT interval
Description of Selected Adverse Reactions Luminous phenomena (phosphenes) were reported by 14.5% of patients, described as a transient enhanced brightness in a limited area of the visual field. They are usually triggered by sudden variations in light intensity. Phosphenes may also be described as a halo, image decomposition (stroboscopic or kaleidoscopic effects), colored bright lights, or multiple image (retinal persistency). The onset of phosphenes is generally within the first two months of treatment after which they may occur repeatedly. Phosphenes were generally reported to be of mild to moderate intensity. All phosphenes resolved during or after treatment, of which a majority (77.5%) resolved during treatment. Fewer than 1% of patients changed their daily routine or discontinued the treatment in relation with phosphenes. Bradycardia was reported by 3.3% of patients particularly within the first 2 to 3 months of treatment initiation. 0.5% of patients experienced a severe bradycardia below or equal to 40 bpm.
In the SIGNIFY study atrial fibrillation was observed in 5.3% of patients taking ivabradine compared to 3.8% in the placebo group. In a pooled analysis of all the Phase II/III double blind controlled clinical trials with a duration of at least 3 months including more than 40,000 patients, the incidence of atrial fibrillation was 4.86% in ivabradine treated patients compared to 4.08% in controls, corresponding to a hazard ratio of 1.26, 95% CI [1.15-1.39].
OVERDOSE
Symptoms Overdose may lead to severe and prolonged bradycardia.
Management Severe bradycardia should be treated symptomatically in a specialized environment. In the event of bradycardia with poor hemodynamic tolerance, symptomatic treatment including intravenous beta- stimulating medicinal products such as isoprenaline may be considered. Temporary cardiac electrical pacing may be instituted if required.
Pediatric Population There is no information on overdose with pediatric population.
PHARMACOLOGICAL PROPERTIES
Pharmacodynamics Properties
Pharmacotherapeutic Group: Cardiac therapy, other cardiac preparations.
Mechanism of Action
Ivabradine is a pure heart rate lowering agent, acting by selective and specific inhibition of the cardiac pacemaker if current that controls the spontaneous diastolic depolarization in the sinus node and regulates heart rate. The cardiac effects are specific to the sinus node with no effect on intra-atrial, atrioventricular or intraventricular conduction times, nor on myocardial contractility or ventricular repolarization. Ivabradine can interact also with the retinal current Ih which closely resembles cardiac If. It participates in the temporal resolution of the visual system, by curtailing the retinal response to bright light stimuli. Under triggering circumstances (e.g. rapid changes in luminosity), partial inhibition of Ih by ivabradine underlies the luminous phenomena that may be occasionally experienced by patients. Luminous phenomena (phosphenes) are described as a transient enhanced brightness in a limited area of the visual field.
Pharmacodynamics Effects The main pharmacodynamics property of ivabradine in humans is a specific dose dependent reduction in heart rate. Analysis of heart rate reduction with doses up to 20 mg twice daily indicates a trend towards a plateau effect which is consistent with a reduced risk of severe bradycardia below 40 bpm. At usual recommended doses, heart rate reduction is approximately 10 bpm at rest and during exercise. This leads to a reduction in cardiac workload and myocardial oxygen consumption. Ivabradine does not influence intracardiac conduction, contractility (no negative inotropic effect) or ventricular repolarization: o In clinical electrophysiology studies, ivabradine had no effect on atrioventricular or intraventricular conduction times or corrected QT intervals; o In patients with left ventricular dysfunction (left ventricular ejection fraction (LVEF) between 30 and 45%), ivabradine did not have any deleterious influence on LVEF.
Pharmacokinetic Properties
Under physiological conditions, ivabradine is rapidly released from tablets and is highly watersoluble (>10 mg/ml). Ivabradine is the S-enantiomer with no bioconversion demonstrated in vivo. The N- desmethylated derivative of ivabradine has been identified as the main active metabolite in humans.
Absorption and Bioavailability
Ivabradine is rapidly and almost completely absorbed after oral administration with a peak plasma level reached in about 1 hour under fasting condition. The absolute bioavailability of the film-coated tablets is around 40%, due to first-pass effect in the gut and liver.
Food delayed absorption by approximately 1 hour, and increased plasma exposure by 20 to 30 %. The intake of the tablet during meals is recommended in order to decrease intra-individual variability in exposure.
Distribution
Ivabradine is approximately 70% plasma protein bound and the volume of distribution at steadystate is close to 100 l in patients. The maximum plasma concentration following chronic administration at the recommended dose of 5 mg twice daily is 22 ng/ml (CV=29%). The average plasma concentration is 10 ng/ml (CV=38%) at steady-state.
Biotransformation
Ivabradine is extensively metabolized by the liver and the gut by oxidation through cytochrome P450 3A4 (CYP3A4) only. The major active metabolite is the N-desmethylated derivative (S 18982) with an exposure about 40% of that of the parent compound. The metabolism of this active metabolite also involves CYP3A4. Ivabradine has low affinity for CYP3A4, shows no clinically relevant CYP3A4 induction or inhibition and is therefore unlikely to modify CYP3A4 substrate metabolism or plasma concentrations. Inversely, potent inhibitors and inducers may substantially affect ivabradine plasma concentrations.
Elimination
Ivabradine is eliminated with a main half-life of 2 hours (70-75% of the AUC) in plasma and an effective half-life of 11 hours. The total clearance is about 400 ml/min and the renal clearance is about 70 ml/min. Excretion of metabolites occurs to a similar extent via faces and urine. About 4% of an oral dose is excreted unchanged in urine.
Linearity/Non-Linearity The kinetics of ivabradine is linear over an oral dose range of 0.5 – 24 mg.
Special Populations
o Elderly: no pharmacokinetic differences (AUC and Cmax) have been observed between elderly (≥ 65 years) or very elderly patients (≥ 75 years) and the overall population.
o Renal Impairment: The impact of renal impairment (creatinine clearance from 15 to 60 ml/min) on ivabradine pharmacokinetic is minimal, in relation with the low contribution of renal clearance (about 20 %) to total elimination for both ivabradine and its main metabolite S 18982.
o Hepatic Impairment: In patients with mild hepatic impairment (Child Pugh score up to 7) unbound AUC of ivabradine and the main active metabolite were about 20% higher than in subjects with normal hepatic function. Data are insufficient to draw conclusions in patients with moderate hepatic impairment. No data are available in patients with severe hepatic impairment.
o Pediatric Population: The pharmacokinetic profile of ivabradine in pediatric chronic heart failure patients aged 6 months to less than 18 years is similar to the pharmacokinetics described in adults when a titration scheme based on age and weight is applied.
Pharmacokinetic/Pharmacodynamics (PK/PD) Relationship PK/PD relationship analysis has shown that heart rate decreases almost linearly with increasing ivabradine and S 18982 plasma concentrations for doses of up to 15-20 mg twice daily. At higher doses, the decrease in heart rate is no longer proportional to ivabradine plasma concentrations and tends to reach a plateau. High exposures to ivabradine that may occur when ivabradine is given in combination with strong CYP3A4 inhibitors may result in an excessive decrease in heart rate although this risk is reduced with moderate CYP3A4 inhibitors. The PK/PD relationship of ivabradine in pediatric chronic heart failure patients aged 6 months to less than 18 years is similar to the PK/PD relationship described in adults.
Preclinical Safety Data
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity, carcinogenic potential. Reproductive toxicity studies showed no effect of ivabradine on fertility in male and female rats. When pregnant animals were treated during organogenesis at exposures close to therapeutic doses, there was a higher incidence of fetuses with cardiac defects in the rat and a small number of fetuses with ectrodactylia in the rabbit. In dogs given ivabradine (doses of 2, 7 or 24 mg/kg/day) for one year, reversible changes in retinal function were observed but were not associated with any damage to ocular structures. These data are consistent with the pharmacological effect of ivabradine related to its interaction with hyperpolarization-activated Ih currents in the retina, which share extensive homology with the cardiac pacemaker if current.
Special Precautions for Storage
This medicinal product does not require any special storage conditions.