

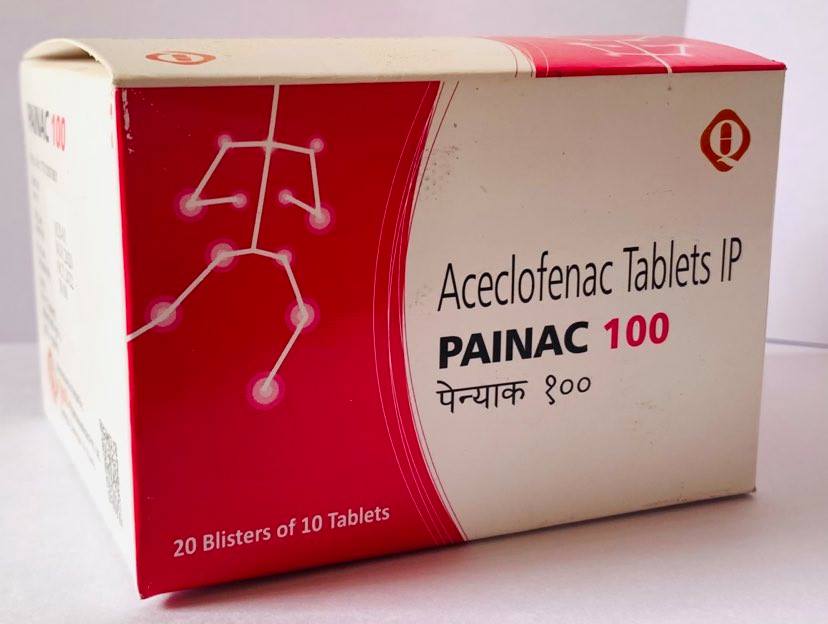
PAINAC 100/ 200 SR
PAINAC contains Aceclofenac 100 /200 mg film-coated Tablets
PRESENTATION
Each tablet contains 100 mg of Aceclofenac film coated tablets.
PHARMACOLOGICAL PROPERTIES
Aceclofenac is a non-steroidal agent with marked anti-inflammatory and analgesic properties. The mode of action of aceclofenac is largely based on the inhibition to prostaglandin synthesis. Aceclofenac is a potent inhibitor of the enzyme cyclooxygenase, which is involved in the production of prostaglandins.
After oral administration, aceclofenac is rapidly and completely absorbed as unchanged drug. Peak plasma concentrations are reached approximately 1.25 to 3.00 hours following ingestion. Aceclofenac penetrates into the synovial fluid, where the concentrations reach approximately 57% of those in plasma. The volume of distribution is approximately 25 L. The mean plasma elimination half-life is around 4 hours. Aceclofenac is highly protein- bound (>99%). Aceclofenac circulates mainly as unchanged drug. 4'- hydroxyaceclofenac is the main metabolite detected in plasma. Approximately two- thirds of the administered dose is excreted via the urine, mainly as hydroxyl metabolites.
No changes in the pharmacokinetics of aceclofenac have been detected in the elderly.
The results from preclinical studies conducted with aceclofenac are consistent with those expected for NSAIDs. The principal target organ was the gastro-intestinal tract. No unexpected findings were recorded. Aceclofenac was not considered to have any mutagenic activity in three in vitro studies and an in vivo study in the mouse. Aceclofenac was not found to be carcinogenic in either the mouse or rat. Animal studies indicate that there was no evidence of teratogenesis in rats although the systemic exposure was low and in rabbits, treatment with aceclofenac (10 mg/kg/day) resulted in a series of morphological changes in some fetuses.
INTERACTION WITH OTHER MEDICINAL PRODUCTS AND OTHER FORMS OF INTERACTION
Other analgesics including cyclooxygenase-2 selective inhibitors: Avoid concomitant use of two or more NSAIDs (including aspirin) as this may increase the risk of adverse effects including GI bleeding. Anti-hypertensive: NSAIDs, may reduce the effect of activity antihypertensive. The risk of acute renal insufficiency which is usually reversible, may be increased in some patients with compromised renal function (e.g. dehydrated patients or elderly patients) when ACE- inhibitors or angiotensin II receptor antagonists are combined with NSAIDs. Therefore, the combination should be administered with caution, especially in the elderly. Patients should be adequately hydrated and consideration should be given to monitoring of renal function after initiation of concomitant therapy, and periodically thereafter.
CLINICAL PARTICULARS
Therapeutic Indications
Aceclofenac film-coated tablets are indicated for the relief of pain and inflammation in osteoarthritis, rheumatoid arthritis and ankylosing spondylitis.
Posology and Method of Administration
Aceclofenac film-coated tablets are supplied for oral administration and should be swallowed whole with a sufficient quantity of liquid.
To be taken preferably with or after food. When Aceclofenac was administered to fasting and fed healthy volunteers only the rate and not the extent of aceclofenac absorption was affected.
Undesirable effects may be minimized by using the lowest effective dose for the shortest duration necessary to control symptoms.
Adults
The recommended dose is 200 mg daily, taken as two separate 100 mg doses, one tablet in the morning and one in the evening.
There are no clinical data on the use of Aceclofenac in children and therefore it is not recommended for use in children under 18 years of age.
The elderly, who are more likely to be suffering from impaired renal, cardiovascular or hepatic function and receiving concomitant medication, are at increased risk of serious consequences of adverse reactions. If an NSAID is considered necessary, the lowest effective dose should be used and for the shortest possible duration. The patient should be monitored regularly for GI bleeding during NSAID therapy.
The pharmacokinetics of Aceclofenac are not altered in elderly patients, therefore it is not considered necessary to modify the dose or dose frequency.
There is no evidence that the dosage of Aceclofenac needs to be modified in patients with mild renal impairment, but as with other NSAIDs caution should be exercised
There is some evidence that the dose of Aceclofenac should be reduced in patients with hepatic impairment and it is suggested that an initial daily dose of 100 mg be used.
Method of Administration
Swallow the tablet whole with a glass of water. Do not crush or chew the tablets. Never change the dose of your medicine without talking to your doctor first. Continue to take your tablets for as long as your doctor recommends.
SIDE EFFECTS/UNDESIRABLE EFFECTS
Overdose
a) Symptoms
Symptoms include headache, nausea, vomiting, epigastric pain, gastrointestinal irritation, gastrointestinal bleeding, rarely diarrhea, disorientation, excitation, coma, drowsiness, dizziness, tinnitus, hypotension, respiratory depression, fainting, occasionally and convulsions. In cases of significant poisoning acute renal failure and liver damage are possible.
b) Therapeutic measure:
Patients should be treated symptomatically as required. Within one hour of ingestion of a potentially toxic amount, activated charcoal should be considered. Alternatively, in adults, gastric lavage should be considered within one hour of ingestion of a potentially life-threatening overdose.
Specific therapies such as, dialysis or haemoperfusion are probable of no help in eliminating NSAIDs due to their high rate of protein binding and extensive metabolism. Good urine output should be ensured. Renal and liver function should be closely monitored. Patients should be observed for at least four hours after ingestion of potentially toxic amounts. In case of frequent or prolonged convulsions, patients should be treated with intravenous diazepam. Other measures may be indicated by the patient's clinical condition. Management of acute poisoning with oral aceclofenac essentially consists of supportive and symptomatic measures for complications such as hypotension, renal failure, convulsions, gastro-intestinal irritation, and respiratory depression.
No changes in the pharmacokinetics of aceclofenac have been detected in the elderly.
SPECIAL WARNINGS AND PRECAUTIONS FOR USE
Undesirable effects may be minimized by using the lowest effective dose for the shortest duration necessary to control symptoms. The use of Aceclofenac with concomitant NSAIDs including cyclooxygenase- 2 selective inhibitors should be avoided.
The elderly have an increased frequency of adverse reactions to NSAIDs especially gastrointestinal bleeding and perforation which may be fatal.
Caution is required if administered to patients suffering from, or with a previous history of, bronchial asthma since NSAIDs have been reported to precipitate bronchospasm in such patients.
Patients with mild to moderate renal impairment should be kept under surveillance, since the use of NSAIDs may result in deterioration of renal function. The lowest effective dose should be used and renal function monitored regularly. Effects on renal function are usually reversible on withdrawal of Aceclofenac.
If abnormal liver function tests persist or worsen, clinical signs or symptoms consistent with liver disease develop or if other manifestations occur (eosinophilia, rash), Aceclofenac Tablets should be discontinued. Close medical surveillance is necessary in patients suffering from mild to moderate impairment of hepatic function. Hepatitis may occur without prodromal symptoms.
Use of Aceclofenac in patients with hepatic porphyria may trigger an attack.
Appropriate monitoring and advice are required for patients with a history of hypertension and/or mild to moderate congestive heart failure as fluid retention and edema have been reported in association with NSAID therapy. Patients with congestive heart failure ( NYHA-I) and patients with significant risk factors for cardiovascular events (e.g. hypertension, hyperlipidemia, diabetes mellitus, smoking) should only be treated with aceclofenac after careful consideration. As the cardiovascular risks of aceclofenac may increase with dose and duration of exposure, the shortest duration possible and the lowest effective daily dose should be used. The patient's need for symptomatic relief and response to therapy should be re- evaluated periodically. Aceclofenac should also be administered with caution and under close medical surveillance to patients with a history of cerebrovascular bleeding.
GI bleeding, ulceration or perforation, which can be fatal, has been reported with all NSAIDs at any time during treatment, with or without warning symptoms or a previous history of serious GI events. Close medical surveillance is imperative in patients with symptoms indicative of gastro-intestinal disorders involving either the upper or lower gastrointestinal tract, with a history suggestive of gastro-intestinal ulceration, bleeding or perforation, with ulcerative colitis or with Crohn's disease, or hematological abnormalities, as these conditions may be exacerbated
The risk of GI bleeding, ulceration or perforation is higher with increasing NSAID doses, in patients with a history of ulcer, particularly if complicated with haemorrhage or perforation, and in the elderly. These patients should commence treatment on the lowest dose available. Combination therapy with protective agents (e.g. misoprostol or proton pump inhibitors) should be considered for these patients, and also for patients requiring concomitant low dose aspirin, or other drugs likely to increase gastrointestinal risk. Patients with a history of GI toxicity, particularly when elderly, should report any unusual abdominal symptoms (especially GI bleeding) particularly in the initial stages of treatment.
Caution should be advised in patients receiving concomitant medications which could increase the risk of ulceration or bleeding, such as systemic corticosteroids, anticoagulants such as warfarin, selective serotonin-reuptake inhibitors or antiplatelet agents such as aspirin. When GI bleeding or ulceration occurs in patients receiving aceclofenac, the treatment should be withdrawn.
In patients with systemic lupus erythematous (SLE) and mixed connective tissue disorders there may be an increased risk of aseptic meningitis.
Serious skin reactions, some of them fatal, including exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis, have been reported very rarely in association with the use of NSAIDs. Patients appear to be at highest risk for these reactions early in the course of therapy, the onset of the reaction occurring in the majority of cases within the first month of treatment. Aceclofenac should be discontinued at the first appearance of skin rash, mucosal lesions, or any other sign of hypersensitivity. Exceptionally, varicella can trigger serious cutaneous and soft tissues infections complications. To date, the contributing role of NSAIDs in the worsening of these infections cannot be ruled out. Thus, it is advisable to avoid use of Aceclofenac in case of varicella.
As with other NSAIDs, allergic reactions, including anaphylactic/anaphylactic reactions, can also occur without earlier exposure to the drug.
Aceclofenac Tablets may reversibly inhibit platelet aggregation (see section 4.5 anticoagulants under 'Interactions').
All patients who are receiving NSAIDs should be monitored as a precautionary measure e.g. renal, hepatic function (elevation of liver enzymes may occur) and blood counts.
Fertility, Pregnancy and Lactation
There is no information on the use of Aceclofenac during pregnancy. Inhibition of prostaglandin synthesis may adversely affect the pregnancy and/or the embryo/fetal development. Data from epidemiological studies suggest an increased risk of miscarriage, cardiac malformation or gastroschisis after use of prostaglandin synthesis inhibitor in early pregnancy. The absolute risk for cardiovascular malformation was increased from less than 1%, up to approximately 1.5%. The risk is believed to increase with dose and duration of therapy.
In animals, administration of a prostaglandin synthesis inhibitor has been shown to result in increased pre- and post-implantation loss and embryo-foetal lethality. In addition, increased incidences of various malformations, including cardiovascular, have been reported in animals given a prostaglandin synthesis inhibitor during the organogenetic period. During the first and second trimester of pregnancy, Aceclofenac should not be given unless clearly necessary. If Aceclofenac is used by a women attempting to conceive, or during the first and second trimester of pregnancy, the dose should be kept as low and duration of treatment as short as possible.
During the third trimester of pregnancy, all prostaglandin synthesis inhibitors may expose the fetus to:
There is no information on the secretion of Aceclofenac to breast milk, there was however no notable transfer of radio labelled (14C) Aceclofenac to the milk of lactating rats. The use of Aceclofenac Tablets should therefore be avoided in pregnancy and lactation unless the potential benefits to the other outweigh the possible risks to the fetus.
The use of Aceclofenac tablets may impair female fertility and is not recommended in women attempting to conceive. In women who have difficulties conceiving or who are undergoing investigation of infertility withdrawal of Aceclofenac tablets should be considered.
Undesirable effects such as dizziness, vertigo, drowsiness, fatigue, visual disturbances or other central nervous system disorders are possible after taking NSAIDs. If affected, patients should not drive or operate machinery.
CONTRAINDICATIONS